What to Know About Mammography Guidelines
As much as the field of mammography has changed over the last decade, there is one condition that remains constant: Confusion. Among the many voices in the industry, there is little consistency around the recommended protocols for mammography screening. From something as fundamental as the age to initiate screening to its recommended frequency, patients and physicians alike continue to be met with contradictory advice.
Despite the latest advancements in imaging technology and cancer treatment, over 45,000 women succumb annually to breast cancer. What is sorely needed in this paradigm is clarity. The American College of Physicians recently reversed its 2015 stance endorsing annual screenings beginning at age 40, to align its recommendations with the controversial United States Preventive Services Task Force (USPSTF) which promotes screening mammograms every two years beginning at 50. Forthcoming are a few facts that should be highlighted with regards to the USPSTF and the science upon which it based its recommendations:
- The task force is essentially comprised of primary care physicians and epidemiologists. There is not a single breast-focused physician on staff, not a breast radiologist, breast surgeon, or medical oncologist
- The recommendations are based on scientifically flawed studies performed on outdated equipment outside of the US in the late 1980s and 1990s
- More recent studies have confirmed the significant difference in number of lives saved by annual versus biennial screening; a 40% mortality reduction in the annual vs. 23% reduction in the biennial patient subgroups
- One out of six breast cancers is diagnosed in women between the ages of 40 and 49
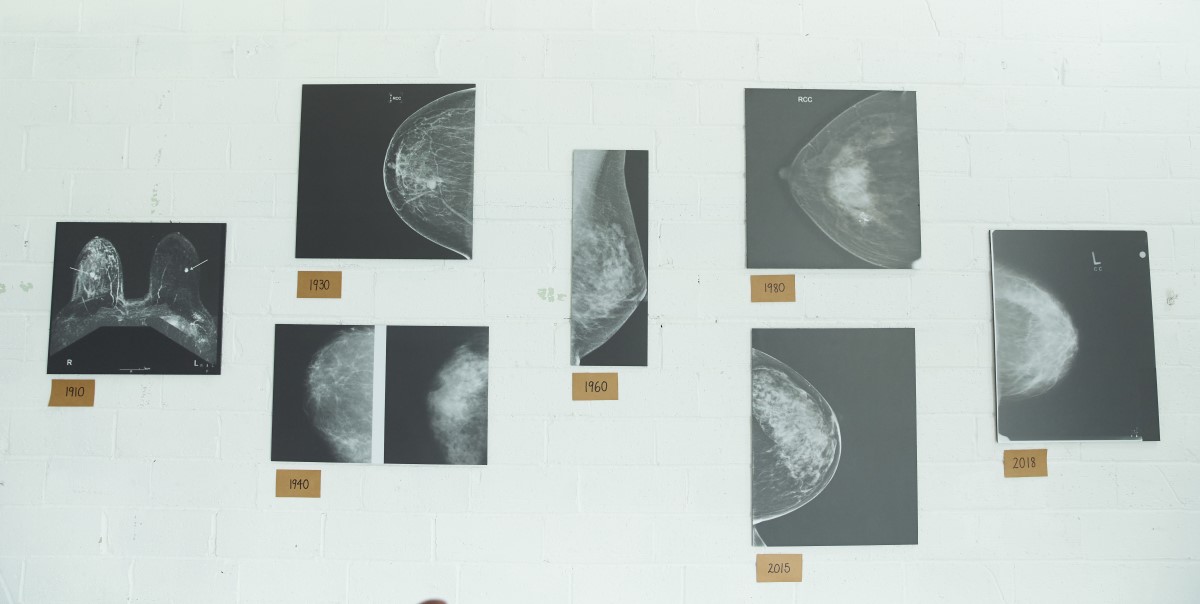
What message is the USPSTF conveying to our younger patient population? The confusion created by this outdated, non-clinically viable data has attempted, and perhaps partially succeeded, in overshadowing the significant progress the field of mammography has made over the last decades; from the advent of digital mammography to the improved accuracy of tomosynthesis (3D) to the game changing comfort of SmartCurve.
Confusion also breeds non-compliance; non-compliance equates to delayed diagnosis, which in turn results in higher treatment costs and decreased life expectancy. At Solis Mammography, we have standardized our care model around annual screenings beginning at age 40 We are anchored to the belief that breast cancer is not preventable, but it is curable if detected early. We are actively engaged in research, education and outreach as we work to perfect the practice of early detection. Our patient-centric emphasis has encouraged us to embark on ground-breaking research collaboratives within the emerging fields of genomic and tumor marker testing. We are hopeful this endeavor will yield a time where screening mammography is no longer needed.