What are Fibrocystic Breasts?
Patients often ask how normal breasts should feel. The truth is that “normal” varies for every woman and every breast. What’s most important is to familiarize yourself with your own body and establish what your breasts feel and look like so that you can easily notice changes.
Fibrocystic breast changes is a common and benign (non-harmful) condition experienced by about half of women. Many women with fibrocystic breasts don’t have symptoms, however some women experience breast pain, tenderness or lumpiness. These changes are normal, but if you find a new or growing lump or skin thickening, worsening of breast pain or changes that persist after your period you should consult your doctor.
Once you familiarize yourself with your normal you will have the power to create lifestyle choices that promote health, healing and self-care. Read on to learn how to live more comfortably with fibrocystic breast change.
Fibrocystic breast changes is a common and benign (non-harmful) condition experienced by about half of women. Many women with fibrocystic breasts don’t have symptoms, however some women experience breast pain, tenderness or lumpiness. These changes are normal, but if you find a new or growing lump or skin thickening, worsening of breast pain or changes that persist after your period you should consult your doctor.
Once you familiarize yourself with your normal you will have the power to create lifestyle choices that promote health, healing and self-care. Read on to learn how to live more comfortably with fibrocystic breast change.
What is fibrocystic breast change?
Fibrocystic breast change affects breast tissue in two ways— by causing thick, scar-like fibrous tissue, called fibrosis, and fluid-filled sacks, called cysts.
Fibrocystic breast symptoms include:
- Breast lumps
- Breast cysts that are round or oval in shape and easily moved
- Breast pain or breast tenderness, especially around your period
- Green or dark brown fluid discharge leaking from your nipple
- Change in breast size or lumpiness that fluctuate in size with your menstrual cycle
What causes fibrocystic breasts?
We don’t know exactly what causes fibrocystic breasts. Researchers believe one cause may be the hormonal changes you experience each month with your menstrual cycle, and that excess estrogen may be what causes fibrocystic breasts. Researchers suspect it’s also the reason why women develop fibrocystic breasts while on hormone replacement therapy.
When do fibrocystic breasts develop in women? Can you have the condition after menopause?
Most women diagnosed with fibrocystic breasts are between 20 and 50. Fibrocystic breasts after menopause are rare because post-menopausal women experience fewer hormonal fluctuations. The exception is women on estrogen replacement therapy. These women sometimes experience a recurrence of their fibrocystic breast symptoms, or even develop them for the first time.
How do you treat fibrocystic breasts?
There’s no cure for fibrocystic breasts, but there’s also no reason to suffer. If your symptoms are disruptive, you and your doctor can customize a treatment plan that makes you more comfortable.
The first and most important step is to understand your symptoms, risks and diagnosis. If you find unusual lumps, pain, tenderness, or discharge during a self-exam, talk to your doctor about your symptoms.
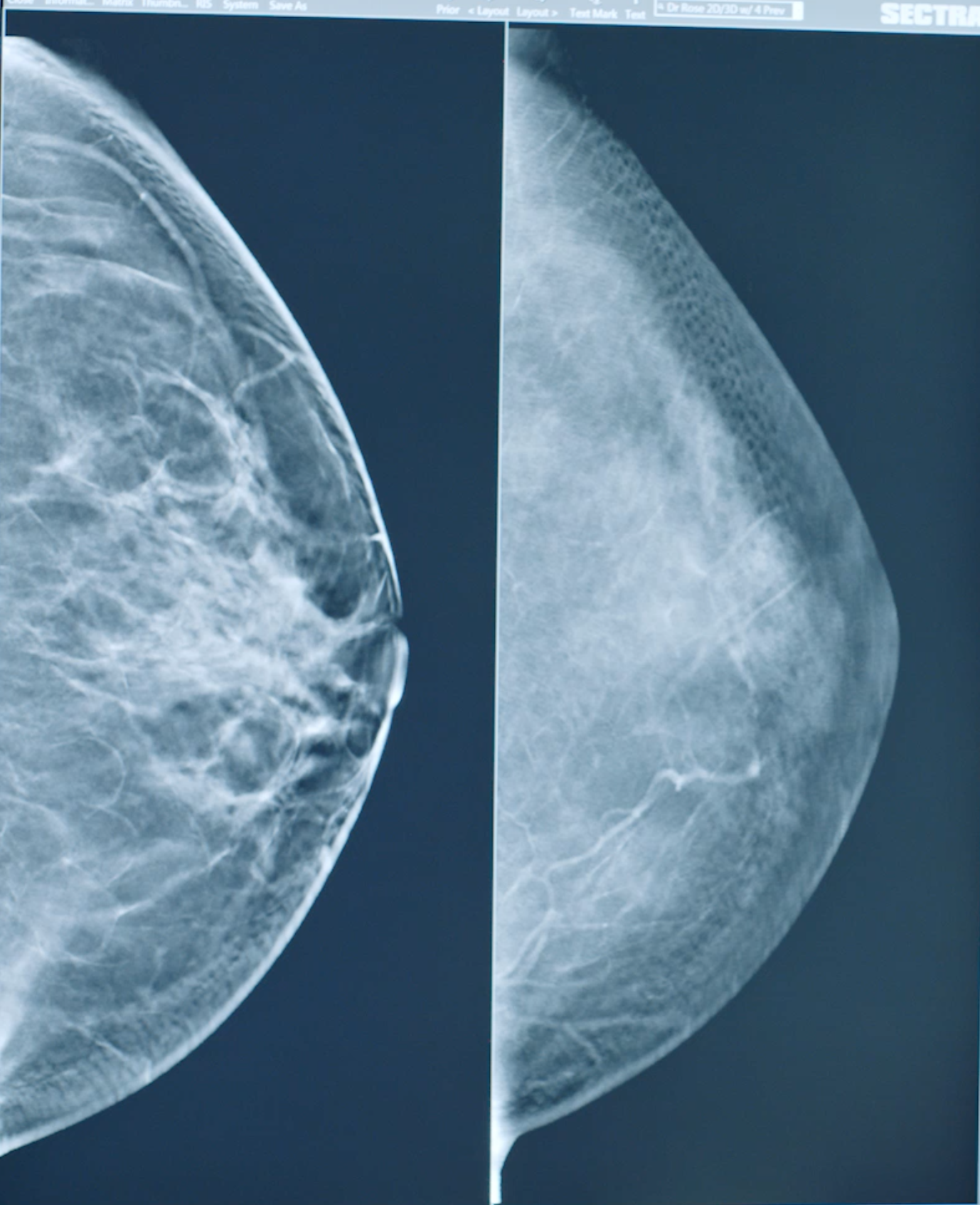
Taking care of yourself and your breasts means annual screening mammograms and clinical breast exams if you’re age 40 or over. Your doctor might order a diagnostic mammogram or an additional screening, like an ultrasound, to better screen for cancers, which can look similar to fibrous breast tissue on a mammogram.
Can fibrocystic breasts lead to cancer?
Though it’s tempting to panic when you feel cysts in your breasts, fibrocystic breast change is not cancer and does not increase your risk of cancer. Dense breast tissue, which sometimes accompanies fibrocystic changes, has been linked to an increased risk of cancer, however.
How long do breast cysts last?
Cysts tend to increase in size or flare up about one week before your period, during what’s called the luteal phase. In most cases, breast cysts and breast pain will resolve once you start your period. If you feel a lump or mass that is accompanied by symptoms such as nipple discharge, rash, swelling, breast warmth, dimpling or puckering of the skin - contact your doctor.
Mammogram for fibrocystic breast tissue
If you’re diagnosed with fibrocystic breasts, your doctor might order a diagnostic mammogram. If you’re already dealing with pain or discomfort from breast cysts, a mammogram might sound like the most painful thing in the world. Solis Mammography adopted the revolutionary SmartCurve technology, which is clinically proven to deliver a more comfortable mammogram for women who have had painful mammograms in the past and provides the advanced accuracy of 3D mammography.
Think of your mammogram as a form of self-care, a way to continue taking care of you.
How to treat pain from fibrocystic breasts
Treatment for fibrocystic breast pain depends on your level of discomfort. For many women, the pain is mild and brief. This is called cyclic pain and usually flares right before you start your period.
In the short-term, an over-the-counter anti-inflammatory like ibuprofen can relieve your swelling and reduce your pain. Your doctor may also prescribe a low-estrogen oral birth control or a progesterone treatment, since high levels of estrogen have been linked to fibrocystic breasts. Natural remedies may also provide relief. Note: Discuss any at-home remedies or supplements with your doctor prior to adding them to your health routine.
Remedies for fibrocystic breast pain:
- Wear a bra that’s supportive but not too tight. If you plan to exercise, pick a sports bra that is comfortably supportive without being constricting.
- Reduce your caffeine intake. There’s been no conclusive link between breast pain and caffeine, but anecdotal evidence supports cutting it out. It’s worth trying if you are experiencing pain and are willing to give up your coffee, tea and chocolate.
- Researchers have explored the idea that maintaining a healthy weight with a low-fat, high fiber diet might help breast pain.
- Supplements with certain vitamins or herbs
- Apply a hot compress or hot water bottle to your breasts to reduce swelling and ease your discomfort.
If breast cysts become too large and painful, your doctor may also choose to drain them, or in very rare cases, to remove them.
Most importantly, you are your best health advocate. Talk with your doctor if you notice any sudden or recurring changes in your breasts so that they can partner with you on the best course of action.